Stroke Education For General Public
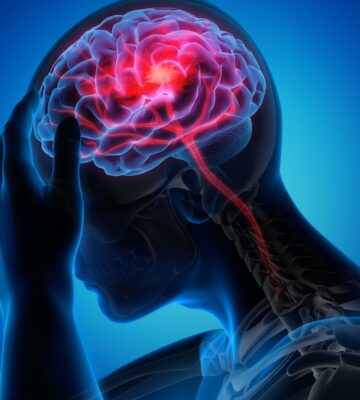
Stroke
A Medical Emergency
Balance loss
Eye disturbances
Facial drooping
Arm weakness
Slurred speech
Time to act fast
For every minute a stroke goes untreated, the brain loses 1.9 million cells. Immediate care at a capable stroke center can drastically improve outcomes. Time saved is brain saved.

What is stroke?
A stroke occurs when blood flow to a part of the brain is interrupted, either due to a blocked artery (ischemic stroke) or a ruptured blood vessel (hemorrhagic stroke). In the context of the PDF, Acute Ischemic Stroke (AIS) is emphasized — this is the most common type, caused by obstruction of cerebral arteries, leading to brain tissue damage due to lack of oxygen. When this happens, brain cells begin to die within minutes.
What is stroke?
As per the TOAST classification, ischemic stroke is categorized into
- Large-Artery Atherosclerosis (LAA)
- Cardioembolic Stroke (CE)
- Small-Vessel Disease (SVD) / Lacunar Stroke
- Stroke of Other Determined Etiology (e.g., vasculitis, dissection)
- Stroke of Undetermined Etiology (Cryptogenic)
Each type has unique causes, such as atherosclerosis, heart disease (especially atrial fibrillation), or small vessel damage due to hypertension or diabetes.
Other types of stroke, each caused by different problems affecting blood flow to the brain:
Ischemic Stroke (Most Common – ~87% of strokes): –
A blood clot or narrowed artery blocks blood flow to the brain.
Subtypes:
- Thrombotic stroke: Clot forms in a blood vessel inside the brain.
- Embolic stroke: Clot or debris forms elsewhere (e.g., heart) and travels to the brain.
Hemorrhagic Stroke: –
A blood vessel in the brain ruptures, causing bleeding into or around the brain.
Subtypes:
- Intracerebral hemorrhage: Bleeding within the brain tissue.
- Subarachnoid hemorrhage: Bleeding into the space between the brain and skull (often from an aneurysm rupture).
Transient Ischemic Attack (TIA) “Mini-Stroke”
Cause:
- A temporary blockage of blood flow to the brain.
- No permanent damage, but symptoms mimic stroke and resolve within minutes to hours.
Warning Sign: Indicates a high risk of future full stroke. Needs urgent medical attention.
Risk factors of stroke:
modifiable and non-modifiable risk factors
- Non-modifiable: Age (>65), gender (male predominance), ethnicity, genetics, low birth weight, Previous Stroke or TIA.
- Modifiable:
- Hypertension (most common)
- Diabetes Mellitus
- Atrial Fibrillation
- Smoking and alcohol
- Dyslipidemia
- Obesity and sedentary lifestyle
- Heart disease (especially AF and valvular diseases)
- Metabolic syndrome
- Dietary factors and drug abuse.
- Poor Diet
- Physical Inactivity
- High Cholesterol
Who all can get affected by stroke?
- Elderly people (≥65 years) are most commonly affected.
- However, the document also highlights a rising incidence in younger adults (<55 years) due to smoking, obesity, and lifestyle changes.
- Women, particularly post-menopausal, have increased stroke incidence due to loss of estrogen’s vascular protective effect.
- People with Chronic Diseases those with: High blood pressure (hypertension), Diabetes, High cholesterol, Heart diseases (e.g., atrial fibrillation), Obesity, Are at a much higher risk.
- Smokers and Alcohol Users: Tobacco and excessive alcohol damage blood vessels and increase blood pressure and clot formation.
- People with a Sedentary Lifestyle: Lack of physical activity increases risk of stroke-related conditions like obesity and high BP.
- People with a Family History of Stroke: – Genetics plays a role. If close relatives had a stroke, your risk is higher.
Children (Rare but Possible): -Though rare, strokes can also occur in newborns and children, often due to congenital heart defects, blood disorders (like sickle cell disease), or infections.
What is the treatment:
Stroke treatment depends on the type of stroke, time of onset, and the patient’s condition. The goal is to restore blood flow to the brain quickly, minimize brain damage, and improve recovery outcomes.
A. Acute Stroke Treatment
Acute stroke management is a medical emergency. Every minute counts — millions of brain cells die each minute during a stroke. Hence, treatment focuses on reperfusion therapy, where the blocked blood vessel is opened as soon as possible.
There are two main evidence-based treatments for Acute Ischemic Stroke (AIS):
Thrombolysis (Intravenous Thrombolytic Therapy (IV tPA))
Thrombolysis involves the use of a clot-dissolving drug to break down the blood clot blocking the brain artery.
The drug used is usually:
rtPA (recombinant tissue plasminogen activator) — commonly Alteplase.
Must be given within 4.5 hours of symptom onset. Earlier administration improves outcomes significantly. The rtPA activates plasminogen in the blood, converting it to plasmin. Plasmin breaks down fibrin, the main component of blood clots.
A patient can receive IV thrombolysis if:
o Stroke onset is within 4.5 hour.
o CT scan rules out bleeding.
o No recent surgery or bleeding disorder.
o Blood pressure is controlled (≤185/110 mmHg).
Benefits:
o Increases chance of complete or partial recovery
o Reduces the size of the stroke and brain damage
o Improves chances of walking independently again
Risks:
o Bleeding in the brain (symptomatic intracranial hemorrhage)
o Should be administered only in stroke-ready hospitals
Thrombolysis (Intravenous Thrombolytic Therapy (IV tPA))
Mechanical thrombectomy is a minimally invasive surgical procedure where a blood clot is physically removed from the brain artery using a catheter-based device. Ideally within 6 hours of stroke onset. Can be done up to 24 hours in selected patients (based on advanced imaging showing salvageable brain tissue).
A catheter is inserted through a groin or wrist artery. It is navigated to the brain artery where the clot is located. A stent retriever or suction device grabs or aspirates the clot. Blood flow is restored to the affected brain area.
Benefits:
o Highly effective in restoring blood flow in major strokes
o Increases chance of a good functional outcome
o Reduces risk of death and long-term disability
Works even when IV tPA is contraindicated or fails
Risks:
o Bleeding at catheter site or in the brain
o Blood vessel injury
o May not be successful in all patients
o Requires specialized stroke intervention team and hospital infrastructure
Supportive Care
Supportive care is the foundation of stroke management, especially in the early hours and days after stroke onset. While advanced treatments like thrombolysis and thrombectomy target the clot directly, supportive care ensures the patient remains stable and safe, preventing complications and improving recovery chances.
Thrombolysis (Intravenous Thrombolytic Therapy (IV tPA))
- Airway and Breathing
- Patients with decreased consciousness or impaired swallowing may need oxygen therapy or even mechanical ventilation to maintain oxygen supply to the brain.
- Oxygen saturation should be kept above 94%.
- Blood Pressure Management
- High blood pressure is common during stroke. For patients not eligible for thrombolysis, BP up to 220/120 mmHg may be allowed (permissive hypertension).
- For those receiving IV thrombolysis, BP must be reduced to ≤185/110 mmHg before treatment to reduce the risk of bleeding.
- Blood Sugar Control
- Both hypoglycemia (<60 mg/dL) and hyperglycemia (>180 mg/dL) can worsen brain injury.
- Blood sugar should be maintained between 140–180 mg/dL using insulin if needed.
- Fever Control
- Elevated temperature increases brain injury, so antipyretics (like paracetamol) should be used to manage fever.
- Hydration and Nutrition
- IV fluids (e.g., normal saline) may be given carefully to prevent dehydration without causing fluid overload.
- Nutrition via feeding tubes may be needed for patients with swallowing difficulty.
- Infection Prevention
- Stroke patients are at risk of pneumonia, urinary infections, and bedsores.
- Early mobilization and proper nursing care are crucial.
- Seizure Management
- Seizures may occur post-stroke. If they do, antiepileptic drugs may be started.
Antiplatelet/Anticoagulant therapy
These therapies are critical for preventing further clot formation and reducing the risk of recurrence, depending on the type and cause of stroke.
Antiplatelet Therapy: Indicated for: Non-cardioembolic ischemic stroke (e.g., caused by large artery atherosclerosis or small vessel disease).
Common drugs: Aspirin (160–325 mg/day), started within 24–48 hours of symptom onset.
In high-risk or minor strokes, dual antiplatelet therapy (DAPT) using aspirin and clopidogrel for 21 days can reduce early recurrence.
Long-term: Usually, single antiplatelet therapy is continued for long-term prevention.
Anticoagulant Therapy: Indicated for: Cardioembolic strokes, especially due to atrial fibrillation (AF).
Common drugs: Warfarin (requires INR monitoring), Direct Oral Anticoagulants (DOACs) like apixaban, rivaroxaban, or dabigatran.
Initiation timing: To avoid bleeding risk, anticoagulants are usually started 4–14 days after stroke, based on infarct size and bleeding risk (follow the “1-3-6-12 day rule”).
Special considerations: Dose adjustment is necessary in elderly or those with kidney disease.
DOACs are preferred over warfarin in most elderly patients due to fewer interactions and lower risk of brain bleeding.
D. Secondary Prevention
Once the immediate danger is controlled, the focus shifts to preventing another stroke, which is called secondary prevention. This is a lifelong process involving medications, lifestyle changes, and monitoring.
Key strategies include:
- Blood Pressure Control: –
Target BP: <140/90 mmHg
Common medications: ACE inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers, diuretics
- Cholesterol Management: –
High-dose statins (e.g., Atorvastatin 40–80 mg) are given to lower LDL cholesterol <70 mg/dL
Statins also stabilize plaques and reduce inflammation
- Diabetes Control: –
Maintain fasting glucose and HbA1c in target range
Use metformin or insulin if needed under medical supervision
- Antiplatelet or Anticoagulant Continuation: –
Based on stroke type and individual risk profile
Lifelong aspirin or DOACs may be continued
- Lifestyle Modifications
Quit smoking and alcohol
Regular physical activity (30 min/day, 5 days/week)
Healthy diet: low in saturated fats and salt, high in fruits and vegetables (e.g., Mediterranean diet)
Maintain healthy weight and waist circumference
- Monitoring and Follow-up: –
Regular visits to monitor BP, cholesterol, blood sugar, and medication side effect.
Echocardiogram, ECG, and Holter monitoring may be done to detect hidden cardiac causes.
- Education and Family Awareness
Teach patients and caregivers about warning signs of stroke (BEFAST)
Encourage early hospital visits if symptoms recur
D. Secondary Prevention
Yes, for secondary prevention, long-term management of risk factors is necessary. This includes:
- Lifelong use of antiplatelets or anticoagulants (based on stroke type)
- Control of BP, glucose, cholesterol
- Lifestyle modifications
- Ongoing physiotherapy or rehab for recovery.
Can we prevent stroke?
Yes, stroke is largely preventable through:
- Effective control of modifiable risk factors (e.g., BP, diabetes, lipids)
- Smoking cessation
- Physical activity.
- Regular health checkups to detect atrial fibrillation and other conditions.
- Eat a Healthy Diet high in: Fruits, vegetables, whole grains, nuts. Low in: Salt, sugar, saturated fats, processed foods.
- Maintain a Healthy Weight: reduces risk of diabetes, high BP, and heart disease.
- Control Heart Problems: atrial fibrillation (AFib) increases clot risk → needs anticoagulants, Regular heart check-ups are important.
- Prevent Transient Ischemic Attacks (TIAs): TIAs (mini-strokes) are warnings — take them seriously, After a TIA, strict prevention is needed to avoid a full stroke.
What is the role of physiotherapy in stroke?
- Physiotherapy is crucial for recovery, especially in elderly.
- It helps with:
- Regaining motor skills, speech, and daily function
- Preventing stiffness, pressure ulcers, and falls
- Enhancing independence and quality of life
- The document emphasizes early, multidisciplinary rehabilitation, which includes physiotherapists, occupational therapists, and speech therapists.
Stages of Physiotherapy:
- Acute Stage : -(Hospital phase)
- Positioning and passive movements to prevent stiffness and bedsores
- Breathing exercises to improve lung capacity
- Begin basic sitting and movement training.
- Subacute Stage (Rehabilitation center or home): –
- Active exercises for weak limbs
- Transfer training (bed to chair)
- Standing and walking practice with aids
- Gait training and balance work
- Chronic Stage (Ongoing rehab at home/clinic): –
- Advanced walking, stairs, coordination, and resistance exercises
- Independence in daily activities
- Long-term strength and endurance building
For any doubts and inquiries, feel free to email us at info@stroke-india.org and our top doctors will respond with expert guidance.